Advance your knowledge
Learn more about wound care
We know how hard it can be to fit continuous learning and development into a nurse’s already busy schedule. That’s why we designed a comprehensive series of digital learning modules that you can use on demand at a time and place that suits you. In many markets, we also offer onsite training and workshops. Reach out to your Mölnlycke representative to learn what is available for you.
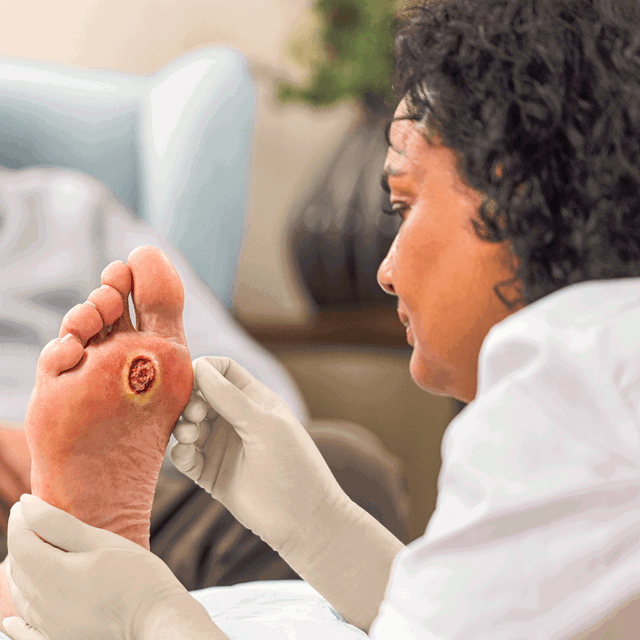
Diabetic foot ulcers - A guide to assessment and management
Your patients with diabetes face challenges every day. We understand how these become your challenges too. Managing long-term conditions involves being able to balance eating, physical activity, medication, and injections. It’s a team effort that can involve a lot of resources and a mix of specialist care.
Talk to our experts
To create a positive impact, we build mutually beneficial relationships with employees, customers and the people in our communities.
Start your conversation hereBuild your learning pathway
The Clinical Learning Hub is the home of educational needs for all levels of healthcare professionals and providers.
Start learning today-
Webinar
Discover webinars packed with valuable information about DFU care. Increase your expertise and enhance your professional development with these informative sessions.
Attend now -
Podcast
Tune into a wealth of podcasts, including several sharing valuable knowledge about DFU care. These insightful episodes will give you a headstart on your professional journey.
Listen now
How to treat diabetic foot ulcers
Diabetic foot ulcers (DFUs) are one of the most serious and costly complications of diabetes, and their prevalence is rising worldwide. We offer solutions to ease the burden of these hard-to-heal ulcers.
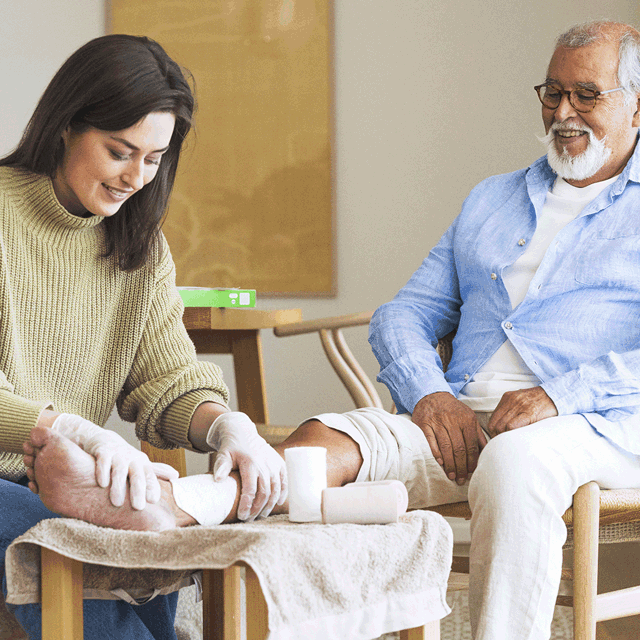
Easy-to-use guides
Provides resources to support nurses, patients, family members and non-medical care givers to confidently manage hard-to-heal wounds at home or in any non-hospital setting.
Related articles
-

Wound care | 5 min read Diabetic foot ulcers: Causes, risks, and epidemiology
Examining the causes, risk factors, and epidemiology of diabetic foot ulcers (DFUs), a serious complication of diabetes, and approaches to prevention and management period.
-

Wound care | 4 min read Diabetic foot ulcers: Treatment, management, and care
Examining how diabetic foot ulcers are diagnosed, treated, and managed, taking a holistic approach to the patient’s individual wound and needs.
-
Wound care | 5 min read Topical oxygen therapy with Granulox™
Watch video





